Clinical Trials - Targeted Solutions:
- Rapid Trial Activation
- Assessment & Roadmap Development
- Clinical Trials Office/Research Operations Office
Research - Targeted Solutions:
Clinical Trials - Targeted Solutions:
- Rapid Trial Activation
- Assessment & Roadmap Development
- Clinical Trials Office/Research Operations Office
Research - Targeted Solutions:
Clinical Trial Site Success: Tackling Challenges in Identification, Selection, Activation, and Ongoing Trials
Introduction
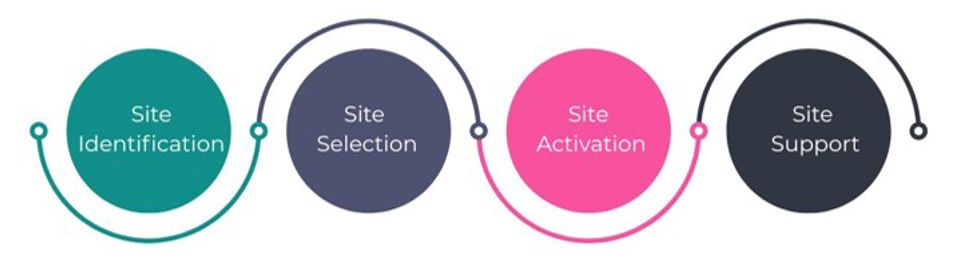
Clinical research sponsors know that the path from identifying an investigative site to running a successful trial is rarely smooth. Each stage of the process (site identification, selection, activation, and ongoing support) brings a unique set of scientific, regulatory, organizational, operational, and business challenges. Overcoming these requires more than clinical research know-how; it calls for business acumen, comprehensive process discipline, and the ability to apply both methodically.

Clinical Trial Site Identification: Data-Driven Site Identification for Faster, Smarter Trials
Challenges in Site Identification
Sponsors often begin the site identification process by casting a wide net, sending feasibility questionnaires to dozens, or even hundreds of potential sites. While this approach may seem thorough, it often results in a flood of inconsistent, incomplete, or unreliable responses. Without a structured, data-driven process for filtering and prioritizing this information, sponsors risk wasting valuable time engaging with sites that may appear promising on paper, but lack the critical elements necessary to deliver, which include access to the right patient populations, reliable infrastructure, operational capacity, or genuine interest and expertise in the study.
The real business challenge here is one of opportunity cost. Every week spent chasing down underqualified or misaligned sites pushes trial timelines further out. That delay has a cascading effect: development costs rise, market competition shifts, and, most importantly, patients in need of new therapies must wait longer for access. In a space where daily burn rates can reach hundreds of thousands of dollars, inefficiency in the earliest stages of site identification is more than just a logistical hiccup; it directly impacts both financial outcomes for sponsors and potentially health outcomes for patients.
How to Improve Clinical Trial Site Identification
This challenge requires both analytical rigor and local insight, including understanding enrollment forecasts, payer landscapes, and competing trial activity while weighing site business models and motivations. Clinical knowledge alone isn’t enough. Business intelligence and operational strategy must be layered into the approach.
Clinical Trial Site Selection: Balancing Science, Operations, and Business Realities
Once a pool of candidate sites has been identified, the next step, site selection, introduces a different set of hurdles.
Pitfalls in Clinical Trial Site Selection
Too often, decisions are influenced by prestige, familiarity, timing of a response, or assumptions rather than objective data. Sponsors may lean toward large academic centers for name recognition, while underestimating smaller community sites that may offer faster access to the right patient populations. At the same time, operational warning signs such as high staff turnover, competing trial commitments, or limited infrastructure may be overlooked. The result is misalignment: sites are chosen that look strong on paper, but ultimately struggle to deliver enrollment, maintain compliance, or keep pace with trial demands.
Balancing Clinical, Business, and Operational Criteria for Site Success
Successful Site Selection requires a thoughtful approach that includes:
- Clinical assessment (disease expertise, PI experience)
- Business assessment (contracting agility, staff stability, financial acumen)
- Operational assessment (availability of dedicated coordinators, efficiency of start-up processes, track record in meeting enrollment targets, and quality of data management practices)
By balancing these perspectives, sponsors can ensure they choose partners who can execute successfully.
Clinical Trial Site Activation: The Biggest Bottleneck in Clinical Research
Site activation remains one of the most significant bottlenecks in clinical research. Data suggests that site activation can account for up to 61% of the total study start-up timeline.[1] A WCG 2024 Clinical Research Site Challenges Survey listed study start-up as the third biggest challenge for sites.[2] While Advarra found that organizations with larger portfolios (300+ industry-sponsored trials) reported turnaround times of 121+ days.[3]
Why Clinical Trial Site Activation Takes So Long
Site activation typically takes so long because it involves a chain of interdependent activities that span multiple domains, including legal, regulatory, financial, clinical, and operational. Contract and budget negotiations alone can take months, particularly at academic medical centers, where numerous institutional site fees and procedural pricing are complex and require multiple rounds of review. At the same time, regulatory and ethics approvals from Institutional Review Boards (IRBs) follow their own schedules and have specific submission requirements, often adding weeks if documents are not prepared meticulously.
Even with this context, 30-40% of sponsors and CROs report they are somewhat or completely unsatisfied with their site initiation process.[4]
Sites also require time to identify the appropriate study team members, conduct training on the protocol, and onboard sponsor-required systems, including data capture platforms and trial portals. Many sites are juggling multiple studies with limited administrative capacity, and the result is a slow process that quickly becomes a bottleneck. Without a structured and proactive approach, these steps stack up, making site activation the single greatest contributor to delays in study start-up.
Each delay has ripple effects: missing the “first patient in” (FPI) date pushes back downstream milestones, increases costs, reduces the time available for recruiting and follow-up, and can lower the morale and commitment at sites, as teams potentially redirect their attention to other trials.
Structured Frameworks that Keep Timelines on Track
During Site Activation, process excellence and project management discipline are as critical as regulatory and clinical expertise. A methodical, documented activation framework reduces back-and-forth and creates accountability, ensuring no step falls through the cracks.
Outsourcing activation to a specialized partner can also give Sponsors and their Site partners greater flexibility and operational bandwidth. By leveraging experienced external teams, organizations can keep timelines moving while scaling resources up or down as trial demands shift, without compromising quality or oversight.
Ongoing Clinical Trial Site Support: Sustaining Performance Across the Clinical Trial Lifecycle
Once a site is activated, the real work begins. Sustaining performance over the life of the trial is rarely straightforward. Sites face ongoing hurdles, including staffing turnover, data entry backlogs, patient recruitment and retention struggles, billing compliance issues, and the potential pressure of competing trials. In addition, sponsors and sites alike struggle with the challenge of forecasting trial resources using traditional methods. Timelines shift, protocols change, and trials themselves are becoming more complex, adding new layers of unpredictability. What appears to be a sufficient staffing plan at study start-up can quickly become inadequate, leaving sites under-resourced and sponsors scrambling to keep studies on track. This dynamic environment makes it nearly impossible to rely on static projections, and without proactive, ongoing support, both operational performance and data quality can suffer.
Sustaining trial performance depends on seamless coordination at the intersection of Sponsors, Sites, and CROs. When these stakeholders operate in sync, sharing visibility, aligning priorities, and anticipating needs, issues can be resolved before they impact timelines or data quality.
Sites without consistent support that spans the lifecycle of the trial face everything from enrollment shortfalls and protocol deviations to costly mid-trial “rescues.”
Continuous Monitoring and Proactive Support to Improve Site Performance
Ongoing support requires continuous business and operational monitoring of the site's financial health, technology adoption, financial tracking and payment processes, alongside clinical oversight. Sustained collaboration, clear communication, and proactive intervention distinguish high-performing sites from those that struggle.
A Holistic View of Clinical Trial Site Success
The four pillars of trial success (Site identification, selection, activation, and ongoing support) are interdependent, with each one shaping the others. A weak identification process leads to poor Site selection; delays in activation, compromised enrollment; and inadequate trial support creates costly mid-trial interventions. The ripple effect is felt across all stakeholders:
- Sponsors absorb higher costs
- CROs struggle to deliver on timelines
- Sites are stretched beyond their capacity.
Ultimately, patients wait longer for new therapies.
These challenges demand a perspective that blends business acumen, operational discipline, and clinical research expertise.
Vitalief brings that unique vantage point. With practical solutions grounded in deep industry experience, we help sponsors, CROs, and sites align their goals, strengthen performance, and keep trials moving forward. By addressing each area methodically while recognizing their interdependence, we enable stakeholders to do more with less and advance clinical research in a way that benefits everyone.
Delays in site identification, selection, activation, and ongoing support are costly and avoidable. Discover how Vitalief helps Sponsors, Sites, and CROs enhance site performance, accelerate timelines, and bring therapies to patients faster.
[1] https://www.appliedclinicaltrialsonline.com/view/fast-tracking-study-start-up-from-site-selection-to-first-patient-enrollment
[2] https://www.wcgclinical.com/wp-content/uploads/2024/12/Decoding-the-Top-Site-Challenges-of-2024-Study-Start-Up-Slides.pdf, p.8
[3] https://www.advarra.com/resources/clinical-trial-activation-sites-infographic/
Schedule a discovery call today!
© 2021-2025 Vitalief. All rights reserved.
Vitalief • New Brunswick, NJ 08901 • United States
By using the website you accept our privacy policy. Choose your cookie consent:

